 Some Canadian researchers believe they may have unlocked part of the mystery of treating anorexia, involving deep brain stimulation.
Some Canadian researchers believe they may have unlocked part of the mystery of treating anorexia, involving deep brain stimulation.
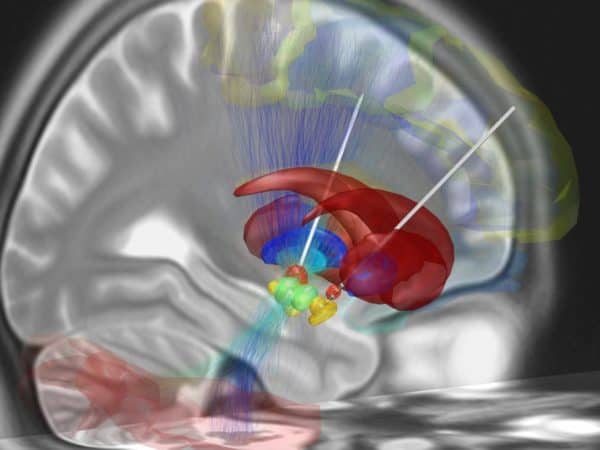
Deep brain stimulation is a surgical technique which involves implanting electrodes into target areas of the brain. First introduced in 1987, the procedure has been applied to a range of illnesses including Parkinson’s disease, Tourette’s syndrome, chronic pain and psychological disorders such as obsessive-compulsive disorder and major depression. Now, researchers at the University of Toronto have shown DBS to be effective in treating anorexia.
While the full explanation of exactly how deep brain stimulation (or DBS) works is still unclear, the basic premise is that by sending regulated electrical impulses to specific regions of the brain, DBS is able to stimulate neuronal activity and induce changes in brain circuitry. “There are circuits in the brain that malfunction, that misfire, and it’s possible to adjust their activity, to turn them up or down, very much like you would adjust the volume on your television set,” says Dr. Andres Lozano of the Division of Neurosurgery at the University of Toronto and co-author of the new study.
For people suffering from the debilitating eating disorder anorexia nervosa, DBS is a new treatment option. The illness itself is often devastating. People suffering from anorexia have a distorted view of their own bodies, an intense fear of gaining weight and go to extreme lengths to control their weight through actions such as binging and purging. Anorexia can lead to death and many suffer for many years despite the best efforts at treatment. Thus, for those with a chronic history of anorexia who have shown a resistance to other treatment option, DBS could stand as a last hope.
“Anorexia remains the psychiatric disorder with the highest mortality rate, and there is an urgent need to develop safe, effective, evidence-driven treatments that are informed by a growing understanding of brain circuitry,” says Dr. Lozano in a release. “Our findings emphasize the need for continued research into novel neuromodulation strategies for anorexia nervosa, and for psychiatric disorders more broadly.”
The small study involved 16 women with a chronic history of anorexia who were given DBS for a one-year period and observed for how well their bodies accepted the surgically implanted electrodes and whether the DBS affected conditions such as body-mass index (BMI), mood, anxiety and anorexia-related behaviours.
For the surgery, while previous research has pinpointed the specific areas of the brain connected to a variety of disorders — in the case of anorexia, it’s the subcallosal cingulate in the cerebral cortex — the exact placement of the electrodes needed to be controlled for each patient, meaning that surgeons require that patients to be awake to provide feedback on changes to thoughts and mood that arise from placing the electrodes in different areas of the brain.
The study results found that while there were some adverse effects of the DBS —two of the 16 patients asked to have their implants removed and one contracted an infection which required another surgery— after one year, the researchers found that mood and anxiety symptoms had been reduced in five patients and depression symptoms in ten, and average BMI of the group increased 3.5 points, with six patients achieving a normal BMI of 18.5 or more.
As well, using PET scans to chart brain activity, the researchers found that after one year of DBS, the areas of the patients’ brains thought to be connected to anorexia had undergone structural changes thought to be improvements in cases of anorexia. “In patients with chronic treatment-refractory anorexia nervosa, DBS is well tolerated and is associated with significant and sustained improvements in affective symptoms, BMI, and changes in neural circuitry at 12 months after surgery,” say the study authors.
The research is published in the journal The Lancet Psychiatry.
Leave a Reply
You must be logged in to post a comment.



 Share
Share Tweet
Tweet Share
Share




Comment